Why This CCO Makes K-Readiness a Priority

Peg King at Health Share’s downtown offices.
Peg King leads Health Share of Oregon’s kindergarten readiness programming. Health Share is the largest Coordinated Care Organization in Oregon, serving approximately 25 percent of the state’s Medicaid patients. It is also one of the most innovative. We talked to King about state health care transformation, Health Share’s commitment to children’s early years, and its burgeoning partnership with Earl Boyles Elementary School in Southeast Portland. We also learned a little bit of Swahili along the way.
CI: What are Coordinated Care Organizations (CCOs)? What is their aim, and to whom are they obligated?
PK: CCOs are private organizations (some are nonprofits, some are not) that contract with the state to coordinate Oregon Health Plan (Medicaid) benefits for OHP members in their local communities. These benefits can include medical, mental health, substance use treatment, dental, and transportation services. Each CCO is different because they each reflect the community they serve, but they all work toward the same goals of better care, smarter spending and healthier people — the Triple Aim.
As a locally owned nonprofit, Health Share’s obligation is first to our members, next to the State of Oregon and its taxpayers, and finally to the providers who serve our members. Health Share works on a local level to ensure Oregon Health Plan members in the tri-county area get the care they need, when they need it. We work with our community to build bridges — connecting our members to services like early learning initiatives, screening and integrated services in maternity care, access to transportation, and more. These connections allow us to hold down costs, improve systems, and quickly identify member and community concerns so we can work together to solve them in a community-based and culturally appropriate way.
CI: Why has Health Share decided to prioritize kindergarten readiness and serving families during the earliest years of a child’s life?
PK: When Oregon signed the Medicaid waiver agreement, the state promised to decrease spending by two percent over five years by improving the way Medicaid services are delivered. To meet this promise, Health Share, like most CCOs, began by addressing the highest utilizing and most costly members. Health Share conducted a qualitative study of these individuals, asking them to describe their lives. The results were really compelling. Most of these members had grown up in chaotic, unstable families. Some had been physically or sexually abused and some had been in and out of the foster care system. Many of them had not finished high school and had more than one chronic physical condition. They did not have childhoods that prepared them to be successful in school or life.
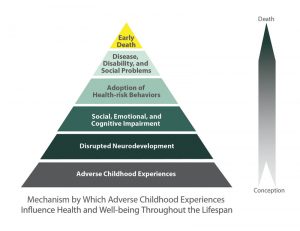
The ACE Pyramid represents the conceptual framework for the ACE Study. The ACE Study has uncovered how ACEs are strongly related to development of risk factors for disease, and well-being throughout the life course.
This all mirrored what we knew from the Adverse Childhood Experiences Study (ACES), published in 1998, that first established the link between toxic stress/childhood adversity and poor mental/physical health in adulthood. The things that derail a healthy life course are often things that are influenced in early life — attachment and bonding, skilled parenting, and social and emotional health. Science now clearly shows that early life adversity impacts the development and architecture of a child’s brain. In the face of such clear evidence, Health Share opted to have a strategic focus on prevention/early life health promotion. By moving our efforts upstream, we hope to improve long-term health outcomes for our members, reduce the number of “high utilizers,” and to ultimately curb Medicaid costs.
CI: What does health look like during the earliest years of a child’s life?
PK: In the early years of a child’s life, you cannot take health and well-being out of the context of the family. Health and well-being means having a stable and nurturing home and neighborhood environment, access to healthy food, and attachment to emotionally healthy parents or caregivers who have the resources, knowledge, and support to meet the child’s needs. Health is much more than just visiting the doctor for check-ups and shots; there is a growing body of research on this. That said, the health care system is sometimes the only system that regularly touches kids before they enter kindergarten, so it is a good place to not only deliver primary care, but to also provide education, parenting support, and referrals to local resources that address the social determinants of health and education.
CI: Why is focusing on prevention unique for a CCO? What shift in thinking does it require?
PK: The focus on prevention is a shift in thinking from traditional managed care. Most health plans and even Medicaid managed care entities are responsible for showing outcomes in the short term. Their job is to manage the “risk” or health outcomes of a certain population of people. Since people switch health plans for all sorts of reasons throughout their life, the incentives for health plans are to keep those people healthy only while they are members of that particular health plan.
Focusing upstream on prevention requires us to think about the community, rather than the CCO, as the entity that is going to receive the return on our investment in the long-term. If we can help support families with young children to create stable environments for their children, then those children will grow up to be healthier, both mentally and physically. Health Share will not likely experience that return on investment for our current members, but future health plans, payers, and the community at large will.
CI: How are you working to identify current gaps in the services your community needs?
PK: Listening and reading! There has been a lot of incredible work done and documented in recent years, including reports, white papers, and community needs assessments. All of this has been of great value. In addition, I spent six months meeting with and listening to dozens of people across multiple systems: primary care, developmental pediatrics, educational service districts, early learning hubs, immigrant and refugee organizations, DHS, parent groups, child-care providers, community-based organizations, home visitors (and more). That is how we know what we don’t know. The best way to figure out what is needed is to go out into the community and listen. At Health Share, we have access to incredibly rich data from our medical claims. We use this to create dashboards and identify trends, gaps, and needs. Healthy equity is a top priority of ours, and our data helps us keep an equity lens on all of our work. Our data is disaggregated by race, ethnicity, and language — among many other factors — so we can identify what populations aren’t being reached and where we might want to focus our efforts.
CI: How are the CCOs and state early learning hubs collaborating?
PK: With recent health and early learning transformation efforts, and overlapping metrics such as developmental screening, the CCOs and state early learning hubs are working more closely and effectively together. It’s exciting to see. The health care and education systems have historically been funded and legislated in silos, so this kind of collaboration is exciting, but can also be difficult and complex. We are all looking for new ways to solve old problems through sharing resources, collaboration and, hopefully, paying for things differently.
At Health Share, we are “buddies” with the three early learning hubs in our region: Washington, Clackamas, and Multnomah counties. There is a joint committee that meets monthly between Family Care (the other CCO in the region), Health Share, and the hubs where we discuss join initiatives and align work.
CI: Tell us a little about the Community Health Worker project Health Share is piloting at Earl Boyles Elementary, one of CI’s Early Works sites.
PK: It is a demonstration project showing how the health and school systems can integrate better to serve families. The goal is to get families that aren’t connected to health services connected. The community health worker at Earl Boyles will build these connections at the school and will also work to build connections with local primary care clinics who house their own community health workers. We are especially excited because it is addressing a community-identified need. I am very encouraged by the idea of schools as community spaces, welcoming spaces where families can connect with each other, the school, and community services. Ensuring kids have all the preventive services by kindergarten is simply a different way of serving our members in a different place (in this case, their neighborhood school) which might be more comfortable and accessible to them.
CI: Why is Health Share interested in lifting up kindergarten readiness and health work to the state policy level?
PK: The science is clear on brain development and early intervention, but policy hasn’t caught up yet.
As the state’s largest CCO, having brought together one of the most diverse sets of stakeholders to focus on transforming health care for Oregon Health Plan (OHP) members, we believe that it is incumbent on us to take a leadership role in setting Medicaid policy for the state. We are in a unique position to view policy issues from a lens of what is best for our members and our community, without regard to the individual interests of any one part of the system. That said, we try to stay focused on OHP-specific issues because that is where our expertise lies.
Policy is ultimately the only way to stabilize a view of the wider system and ensure sustainable funding. There are so many incredible small projects and initiative and great ideas out there, but until we have policies that drive collaboration and systems thinking, it will be hard to find permanent solutions.
CI: What are the biggest gaps you see in the current state health system?
PK: This isn’t really a question Health Share should answer for the state, but we can answer what gaps we’re focused on bridging in our community.
At Health Share, we know that health doesn’t just happen in the doctor’s office — it starts in the community. For all of us, our health depends on where we live, work, play, and go to school. Upstream factors such as access to healthy food, social networks, poverty, and stable housing are just important as quality health care services. By bridging the gaps between health care services and other community-based services (such as education, transportation, etc.), and by partnering with community organizations to build trust and bring services directly to our members, we can help them get the care they need to be healthy and well.

“The lion who moves slowly is the one who eats the meat” is one of Peg’s favorite Swahili phrases. It aligns well with her focus on prevention!
CI: A little bird told us you speak Swahili from your time in the Peace Corps. What is your favorite saying?
PK: Simba mwnda pole ndiye mla nyama. It means, “The lion who moves slowly is the one who eats the meat.”





 This new study, conducted by the Children’s Institute and Chalkboard Project, finds that rural Oregon students face the twin challenges of poverty and distance in meeting their education goals. The study examines how rural students perform compared to their peers in the rest of Oregon and around the country.
This new study, conducted by the Children’s Institute and Chalkboard Project, finds that rural Oregon students face the twin challenges of poverty and distance in meeting their education goals. The study examines how rural students perform compared to their peers in the rest of Oregon and around the country.